Thyroid Nodules
Anatomy and Pathophysiology:
Thyroid masses are common in the adult population. About 4-7% of North Americans have a palpable thyroid nodule. Most nodules, or lumps within the thyroid gland, are benign. This chapter will focus primarily on the evaluation and management of thyroid neoplasms that may require surgical intervention.
The thyroid gland is an endocrine gland located in the midline anterior neck. It is composed of two lateral lobes connected by a central isthmus. In some cases, a third, pyramidal lobe may extend superiorly from the midline or either lateral lobe. The gland is enclosed by layers of deep cervical fascia and is attached to the underlying tracheal rings and cricoid cartilage by the posterior suspensory ligament (ligament of Berry). The arterial supply of the thyroid is via the superior thyroid artery (branch of the external carotid) and inferior thyroid artery (branch of the thyrocervical trunk); venous drainage is via the superior, middle, and inferior thyroid veins.
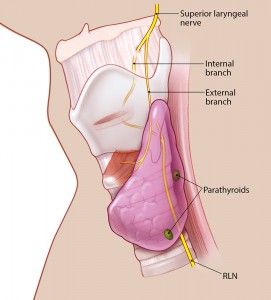
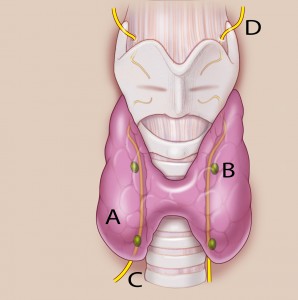
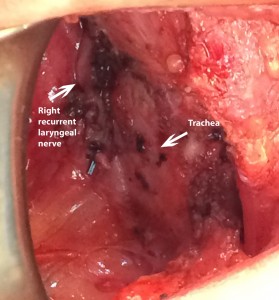
Important anatomical considerations when operating on the thyroid include its relationship to the recurrent and superior laryngeal nerves, which provide innervation to many pharyngeal and laryngeal structures. In the neck, the left recurrent laryngeal nerve (RLN) ascends paratracheally, in close proximity to the tracheoesophageal groove. The right RLN enters the neck more laterally, but travels medially as it ascends.
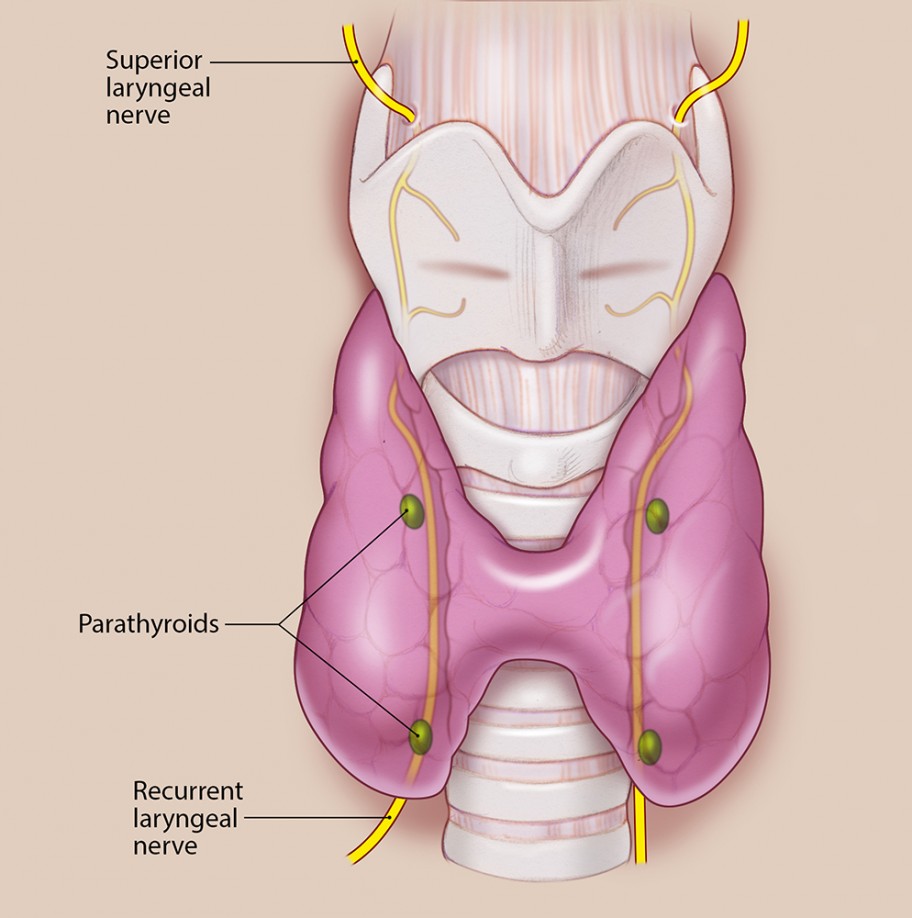
Thyroid gland with right recurrent laryngeal nerve lying more lateral to the trachea compared to the left.
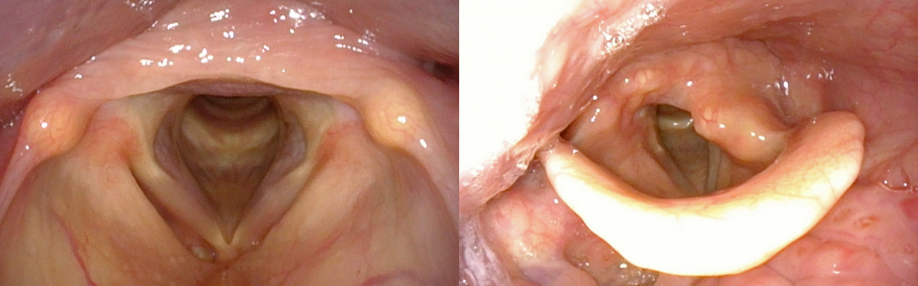
The external branch of the superior laryngeal nerve (SLN) innervates the cricothyroid and inferior constrictor muscles. Part of its course lies in close proximity to the vascular pedicle supplying the superior pole of the thyroid. The external branch of the SLN may thus be injured during ligation of these vessels, resulting in changes to voice quality and vocal range.
Additionally, the parathyroid glands, which regulate calcium levels in the blood, are found posterior to the thyroid gland. Four or more parathyroid glands may be present. As many of the parathyroid glands as possible should be identified and preserved during thyroid surgery to avoid postoperative hypoparathyroidism and hypocalcemia.

Functionally, the thyroid gland produces two hormones, T3 (triiodothyronine) and T4 (thyroxine), which are important for metabolism, growth, and development. Regulation of thyroid hormone production is via secretion of thyroid stimulating hormone (TSH), which is produced by the pituitary gland. Embryologically, the thyroid forms at the base of the tongue and follows a tract of descent into its final position in the neck. Faulty or incomplete migration of the gland can result in lingual (ectopic) thyroid or a thyroglossal duct cyst; the latter is discussed in greater detail in Pediatric Neck Masses.
Epidemiology, Natural History, and Presentation of Common Thyroid Nodules:
The following is a summary of the most commonly encountered thyroid nodules:
Adenoma – This follicular neoplasm is the most common benign thyroid lesion, typically representing 70-80% of thyroid nodules. Incidence is highest in women over the age of 30 years. Often, these nodules are mobile, non-tender and asymptomatic. In a minority of cases, the adenoma may be secreting too much thyroid hormone with the potential of thyrotoxicosis.
Papillary carcinoma – This well-differentiated thyroid follicular malignancy is the most common thyroid cancer. Incidence is highest in females in the fourth to fifth decades of life. In the majority of cases, papillary carcinoma presents as a painless, slow-growing neck mass without functional disturbance. This cancer tends to spread via the lymphatic channels. In more advanced cases, symptoms associated with mass effect and/or extrathyroidal spread may be apparent such as dysphagia or dysphonia.
Follicular carcinoma – This well-differential thyroid carcinoma represents 10-13% of thyroid malignancies. Incidence is highest in middle-aged to elderly women, with a mean age of presentation of 50 years. There is an association with iodine deficiency, and the tumor is more prevalent in areas of endemic goiter. Follicular carcinoma usually presents as a painless, solitary thyroid nodule. Occasionally, patients may present with a sudden increase in size of a longstanding goiter or with thyrotoxicosis. Lymphatic spread is uncommon (greater than 10 percent of cases), but distant metastasis occurs more frequently than in papillary carcinoma. Common sites of distant metastasis include bone, liver, lung, and brain.
Hürthle cell tumor – This follicular neoplasm derives from Hürthle, or oxyphilic, cells of the thyroid. It is usually benign. In about 20% of cases, it is malignant. Tumor nodules may be associated with Hashimoto thyroiditis, Grave’s disease, or multinodular goiter. Hürthle cell carcinomas represent approximately 3% of all thyroid malignancies and are considered more aggressive than follicular carcinoma. Multifocal and bilateral disease is common, as are cervical nodal and distant metastases.
Medullary thyroid carcinoma (MTC) – This malignancy arises from the parafollicular C cells and accounts for approximately 4-5% of thyroid malignancies. More than other types of thyroid cancer, MTC is frequently associated with positive family history (30% of cases). Also unlike other types of thyroid cancer, there is no gender predilection. Incidence is highest in the sixth and seventh decades of life for spontaneous cases, whereas familial cases are diagnosed in younger patients. It has a propensity for both locoregional lymphatic spread and distant metastases, typically the mediastinum, liver, lung, and bone. Due to local nvasion, pain, dysphagia, dyspnea, and/or dysphonia are more common.
Anaplastic (undifferentiated) carcinoma – This is a rare, poorly differentiated cancer accounting for less than 5% of thyroid malignancies, but is notable for their extremely aggressive behavior. Incidence is highest in women between the ages of 60 and 70 years. Up to 80% of cases occur with a synchronous or metachronous carcinoma. Over 80% of cases exhibit locoregional lymphatic spread and 50% present with distant metastases. Typical presentation is with sudden and rapid enlargement of a neck mass. Symptoms of pain, dysphagia, dyspnea, and dysphonia are common.

Differential Diagnosis of Thyroid Mass
- Benign Neoplasm
- Follicular adenoma
- Benign Hürthle cell tumor
- Benign salivary gland neoplasm
- Adenolipoma
- Hyalinizing trabecular tumor
- Paraganglioma
- Teratoma
- Malignant Neoplasm
- Papillary carcinoma
- Follicular carcinoma
- Hürthle cell carcinoma
- Medullary thyroid carcinoma
- Anaplastic carcinoma
- Malignant salivary gland neoplasm
- Squamous cell carcinoma
- Lymphoma
- Small cell carcinoma
- Lymphoma
- Metastasis
- Nonneoplastic
- Hyperplastic goiter
- Thyroid cyst
- Ectopic thyroid
- Chronic thyroiditis
- Riedel thyroiditis
- Amyloid goiter
- Abscess
- Extrathyroidal Etiology
- Parathyroid tumor
- Hyperparathyroidism
Evaluation:
A complete patient history for a complaint of thyroid mass includes assessment of timing of onset and progression, history of ionizing radiation exposure, family history of thyroid disease, and presence of associated symptoms that may indicate extrathyroidal extension (e.g., dysphagia, hoarseness, difficulty breathing). Symptoms of thyroid dysfunction should also be elucidated, including changes in weight, heat or cold intolerance, energy level, and/or appearance of hair/nails/skin. Patients with hypo- or yperthyroidism are more likely to have nonmalignant masses.
A comprehensive head and neck examination should be performed. The thyroid mass should be palpated, noting size, consistency, and mobility. Any involvement of, or fixation to, the overlying skin should be noted. The neck should be thoroughly assessed for cervical lymphadenopathy. A flexible fiberoptic laryngoscopic examination should be performed to assess vocal cord function and/or tumor extension into the larynx.
In regard to laboratory tests, measurement of TSH level is generally sufficient as a screening test for thyroid function. If family history of MTC or MEN is present, or if FNA-C results are suggestive of MTC, calcitonin level should be measured.
Ultrasound of the thyroid is diagnostic imaging of choice at this point. It can be used to determine characterics of thyroid nodules, monitor growth of nodules and assist in biopsy of nodules if needed. In addition, ultrasonography should evaluate for cervical lymphadenopathy in cases of suspected malignancy. The use of computed tomography (CT) and magnetic resonance imaging (MRI) is typically reserved for cases where extrathyroidal extension is suspected.
Fine needle aspiration cytology (FNA-C) is the diagnostic procedure of choice in evaluating thyroid nodules, as it is minimally invasive, can be performed in the office setting, and has a high diagnostic accuracy for certain tumors. Drawbacks to FNA-C include dependence on technical proficiency of the performer and possibility of non-diagnosis despite biopsy.
Up to 15% of aspirate samples are inadequate or nondiagnostic, frequently due to aspiration of cyst fluid or areas of hemorrhage or necrosis. FNA-C results are categorized as benign, malignant, or suspicious, with the suspicious category generally consisting of follicular neoplasms with atypical cytologic features. Although FNA-C is up to 99% accurate in diagnosing papillary thyroid carcinoma, it cannot distinguish between follicular carcinoma and follicular adenoma with atypia. The diagnosis of follicular carcinoma must be made based on histologic features such as capsular invasion or microvascular involvement. The same is true for distinguishing between benign and malignant Hürthle cell tumor. Studies have shown that approximately 20% of cases diagnosed as follicular neoplasm on FNA-C are malignant.

Several tumor staging systems exist for classification of thyroid malignancy, each taking into consideration a different set of evaluation criteria. These include the American Joint Commission on Cancer (AJCC) TNM classification, the AMES system, the AGES system, and the MACIS system. Current American Thyroid Association (ATA) guidelines recommend the use of the AJCC TNM system for staging of well-differentiated thyroid carcinoma; this system is summarized in the table below.
| AJCC TNM Staging System for Well-Differentiated Thyroid Carcinoma | |||
|---|---|---|---|
| Primary Tumor (T) | Regional Lymph Nodes (N) | Distant Metastasis (M) | |
| Tx: cannot assess | Nx: cannot assess | ||
| T0: No evidence of tumor | N0: No regional lymph node metastasis | M0: No distant metastasis | |
| T1a: ≤ 1 cm and limited to the thyroid | N1a: Metastasis to Level VI (pretracheal, paratracheal or prelaryngeal/Delphian lymph nodes) | M1: Distant metastasis | |
| T1b: > 1 cm but ≤ 2 cm and limited to the thyroid | N1b: Metastatis to ipsilateral, contralateral or bilateral lateral lymph nodes (Level I-V) or retropharyngeal or mediastinal lymph nodes | ||
| T2: > 2 cm but ≤ 4 cm without extraparenchymal extension | |||
| T3: > 4 cm or limited extension to sternothyroid muscle or perithyroid soft tissue | |||
| T4a: Invades subcutaneous soft tissues, larynx, trachea, esophagus or recurrent laryngeal nerve | |||
| T4b: Invades prevertebral fascia or encases carotid artery or mediastinal vesse | |||
| Age < 45 years | |||
| Stage 1 | Any T | Any N | M0 |
| Stage 2 | Any T | Any N | M1 |
| Age ≥ 45 year | |||
| Stage I | T1 | N0 | M0 |
| Stage II | T2 | N0 | M0 |
| Stage III | ≤ T3 | ≤ N1a | M0 |
| Stage IVA | ≤ T4a | ≤ N1b | M0 |
| Stage IVB | T4b | Any N | M0 |
| Stage IVC | Any T | Any N | M1 |

Treatment:
Treatment algorithms for the management of thyroid nodules typically hinge on FNA-C results. A benign FNA-C has a low false-negative rate (1-6%) and can be observed. ATA guidelines suggest monitoring with serial clinical examinations and/or ultrasound every 6 to 18 months. Increases in nodule size warrants repeat FNA-C.
Biopsy diagnosis of follicular neoplasm can be managed in multiple ways. In general a thyroidectomy is recommended to determine if the follicular neoplasm is an adenoma or a carcinoma. However, a thyroid lobectomy versus a total thyroidectomy is controversial. Either surgery can be performed. Features concerning for carcinoma include multiple personal or family history risk factors, nodule size greater than 4 cm, extra-thyroidal symptoms and rapid growth. Because of the rarity of lymphatic spread in follicular carcinoma, neck dissection is only performed if there is clinical or radiographic evidence of cervical nodal metastasis. Postoperatively, adjunctive radioactive iodine ablation (RAI) is given depending on the final pathology results.
Currently, for papillary thyroid carcinoma, the general recommendation is a total thyroidectomy. Addition of a mandatory central neck dissection of lymph nodes or an elective dissection has been controversial. Postoperative radioactive iodine (RAI) is typically given. The import of occult/microscopic nodal metastases in papillary carcinoma is unclear, but RAI therapy is thought to address this regardless.
Medullary thyroid carcinoma management involves further studies. Because of the high frequency of familial/genetic etiology in MTC, testing for RET proto-oncogene mutation is often also performed. Positive RET proto-oncogene mutation in family members involves recommendation of a prophylactic total thyroidectomy. Patients should be screened for presence of other associated neoplasms and disorders such as pheochromocytoma or hyperparathyroidism. In general, total thyroidectomy is the recommended treatment. Due to the high rate of cervical nodal metastasis, the neck is usually addressed surgically with bilateral central compartment dissections. Elective ipsilateral dissection of levels II-V is recommended if there are positive central compartment lymph nodes, or if the primary tumor is over 1 cm in size.

Due to extremely aggressive nature of anaplastic carcinoma, treatment is generally palliative. Establishment of a secure airway is the primary concern and generally requires tracheostomy with or without tumor debulking. Chemotherapy and chemoradiation protocols are actively being researched.
Complications, Prognosis and Follow-Up
In cases of total thyroidectomy, postoperative thyroid hormone replacement therapy must be given to avoid symptoms of hypothyroidism.
Radioactive iodine ablation therapy is given in cases of well-differentiated thyroid carcinoma. Because elevated TSH increases radioiodine uptake, suppressive thyroxine therapy must be suspended prior to initiating RAI.
Postoperative surveillance in cases of well-differentiated thyroid carcinoma involves monitoring TSH levels and thyroglobulin. Serum thyroglobulin is produced by thyroid tissue. Hence it is a sensitive indicator of tumor recurrence in the post-thyroidectomy patient. General recommendations suggest measuring thyroglobulin levels every 6-12 months after initial therapy.
The prognosis for papillary thyroid cancer is very good. The five-year survival rate for patients under 45 years of age is 99%, regardless of stage. Survival rate is lower in older patients, 80% overall. Recurrence rates for papillary thyroid carcinoma after total thyroidectomy are reported to be in the range of 10-15%, although tumor recurrence does not appear to be directly related to increased mortality. Poor prognostic indicators in papillary thyroid carcinoma include increased patient age, male sex, extrathyroidal invasion, tumor recurrence, and distant metastases.
Follicular carcinoma has been reported to have higher rates of recurrence, 30%, and lower survival rates, overall 5-year survival of 70%. Poor prognostic factors include age greater than 50 years, tumors larger than 4 cm, extrathyroidal invasion, vascular invasion, and distant metastases.
Medullary thyroid carcinoma is reported to have a 10-year survival rate of 60-75%. Prognosis is directly related to tumor stage. In addition, the presence of cervical nodal metastasis is a poor prognostic indicator. Postoperative surveillance is with the use of serum calcitonin and CEA monitoring.
Anaplastic carcinoma has a poor prognosis, with a median survival of 2 to 6 months after diagnosis. Mortality is generally a result of exsanguination, airway obstruction, or superior vena cava syndrome. Chemotherapeutic regimens produce a reported 2 year survival rate of 12%.
Additional References
Key Points
- Surgical anatomy of the thyroid should include consideration of the recurrent laryngeal nerves, superior laryngeal nerves, and parathyroid glands.
- Fine needle aspiration cytology (FNA-C) is the primary diagnostic modality for thyroid masses; results are categorized as benign, malignant, suspicious, or inadequate/nondiagnostic.
- Thyroid (follicular) adenoma:
- Most common benign thyroid lesion
- FNA-C diagnosis is benign, unless atypia is present (diagnosis is suspicious)
- If FNA-C is benign, lesion may be monitored by serial examination or ultrasound
- FNA-C should be repeated if increase in nodule size is noted
- Papillary carcinoma:
- Most common malignant thyroid tumor
- Multifocal disease and cervical lymph node metastasis are common
- Distant metastasis is present in 10%, most common in the lungs
- FNA-C is very accurate for diagnosis
- Treatment is generally with total thyroidectomy
- Neck dissection is reserved for N1 necks
- Postoperative radioactive iodine (RAI) ablation is standard
- Follicular carcinoma:
- Diagnosis is made on basis of histologic features (e.g., capsular invasion)
- FNA-C cannot make definitive diagnosis
- An FNA-C diagnosis of follicular neoplasm warrants thyroid lobectomy; if surgical pathology reveals malignancy, completion thyroidectomy is then performed and postoperative RAI is given
- Lymphatic spread is uncommon
- Distant metastasis occurs more frequently than in papillary carcinoma (common in bone)
- Hürthle cell carcinoma is a follicular neoplasm that behaves more aggressively than follicular carcinoma
- Medullary thyroid carcinoma (MTC):
- Arises from parafollicular C cells
- Associated with family history/familial conditions in 30% of cases
- FNA-C diagnosis is confirmed by serum calcitonin levels
- Locoregional lymphatic spread and distant metastases are common
- Treatment is with total thyroidectomy and bilateral neck dissection
- RAI is not effective at eliminating residual tumor
- Postoperative surveillance is by monitoring serum calcitonin and CEA
- Anaplastic (undifferentiated) carcinoma:
- Extremely aggressive tumor
- Locoregional lymphatic spread in >80% and distant metastasis in >50% of cases
- No effective treatment modalities; mean survival is 2-6 months after diagnosis
- Chemotherapy with doxorubicin may marginally increase survival rates
- Thyroid hormone replacement therapy is given after total thyroidectomy to avoid symptomatic hypothyroidism.
- Suppressive L-thyroxine therapy is also given to decrease risk of recurrence due to trophic effects of TSH on residual thyroid tissue.