Otitis Media
Definition and Pathophysiology:
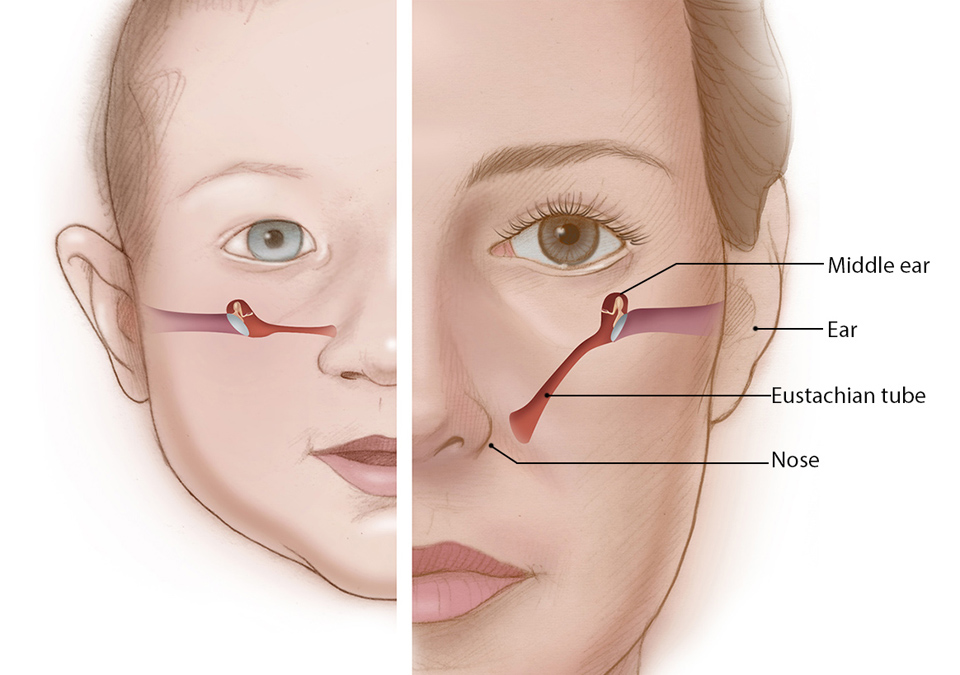
Otitis media is an inflammatory or infection of the middle ear space, which is extremely common, particularly in the pediatric population. The middle ear space is connected to the nasopharynx by the Eustachian tube. This Eustachian tube allows equalization of pressure between the air filled middle ear space and the air filled nasopharynx. If there is dysfunction of the Eustachian tube, the risk of developing infections or inflammation of the middle ear space increases. The relationship of the Eustachian tube to the middle ear space and the air filled nasopharynx. If there is dysfunction of the Eustachian tube, the risk of developing infections or inflammation of the middle ear space increases. The relationship of the Eustachian tube to the middle ear space and nasopharynx changes over the course of development. This change leads to decreased risk of developing otitis media.
Otitis media is divided into two categories: acute otitis media (AOM) and otitis media with effusion (OME). According to the American Academy of Pediatrics clinical practice guideline from 2013, acute otitis media involves otalgia with mild bulging of the tympanic membrane and effusion. According to the clinical practice guideline endorsed by the American Academy of Otolaryngology–Head and Neck Surgery, otitis media with effusion involves middle ear fluid found on pneumatic otoscopy with the absence of acute symptoms.
There are several causes of acute otitis media: viral, bacterial or fungal. Viral upper respiratory infections precede up to half of all cases of AOM. Respiratory syncytial virus is the most commonly implicated virus in AOM. Whether viral antigens play a direct role in causing AOM, aside from their impact on Eustachian tube or mucosal inflammation, is not completely understood. Viruses are not commonly isolated from middle ear aspirates in AOM, but may explain failure of antibiotic therapy in some cases. Furthermore, viral infections can cause or worsen Eustachian tube dysfunction by causing inflammation to the mucosa of the tube. Bacteria may then invade the middle ear space from the nasopharynx and proliferate as a result of inadequate drainage. If there is bacteria, the most common bacterial organisms isolated in AOM are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Otitis media with effusion may have similar bacteria but the proportions of bacteria isolated are quite different.
Common Bacterial Causes of Otitis Media and Mastoiditis
| Condition | Common Causative Organisms | Relative Frequency |
|---|---|---|
| Acute otitis media | Streptococcus pneumoniae Haemophilus influenzae Moraxella catarrhalis | 35% 23% 14% 28% |
| Otitis media with effusion | Other No growth Haemophilus influenze Moraxella catarrhalis | 45% 30% 15% 10% |

Epidemiology:
It is estimated that between 80-90% of children in the United States have had at least one episode of AOM by the age of 3 years. AOM accounts for up to one-third of pediatric office visits. AOM may occur any time after birth, although peak incidence is between the ages of 6 and 12 months. There is an increased occurrence of AOM for children who attend group daycare, have atopy, or are exposed to cigarette smoke. Also, there is a slight predilection for male children. In addition, children with craniofacial anomalies resulting in Eustachian tube dysfunction also have higher rates of infection. AOM can occur in adults but is not as common. According to the American Academy of Otolaryngology–Head and Neck Surgery in 2004, up to 2.2 million children annually develop otitis media with effusion.
Natural History:
Most cases of acute otitis media will resolve spontaneously without treatment. Studies with a placebo control have demonstrated resolution rates of greater than 85% by 7 days in uncomplicated cases of AOM. Despite this, medical therapy is typically given both for symptomatic relief as well as to avoid complications of untreated AOM.
About 70-90% of OME resolves in 3 months without further treatment. However, hearing loss or decrease in development especially in children may lead to intervention such as tympanostomy tubes.
Presentation:
The primary symptoms of AOM in children are otalgia exhibited by holding ear, tugging ear or unconsolable crying with fever. Other symptoms may include irritability, lethargy, sleep disturbance and anorexia. For adults, otalgia is accompanied by decreased hearing from conductive hearing loss and ear fullness or pressure. The presence of fever in AOM is variable. Fever greater than 104°F is unusual and typically signifies additional disease process(es), such as bacteremia or intracranial extension. Concurrent or antecedent symptoms of upper respiratory infection may be present, including rhinorrhea, sore throat, or cough. If the tympanic membrane has ruptured, or if AOM occurs in a patient with tympanostomy tubes in place, purulent otorrhea may be noted.
Patients with otitis media with effusion present more with ear fullness or pressure or clogged feeling of ears with associated hearing loss. Some patients may describe the pressure more as a pain.
There are several causes of ear pain or otalgia including acute otitis media or otitis media with effusion. It is important to keep a wide differential in mind during the work up of otalgia.
Differential Diagnosis of Ear Pain:
- Infectious
- Acute otitis externa
- Chronic otitis externa
- Malignant otitis externa (skull base osteomyelitis)
- Auricular cellulitis
- Auricular chondritis
- Acute otitis media
- Chronic serous otitis media
- Bullous myringitis
- Aural tuberculosis
- Acute mastoiditis
- Neoplasm of the External, Middle, or Inner Ear
- Trauma
- Auricular hematoma
- Canal laceration
- Tympanic membrane perforation
- Temporal bone fracture
- Barotrauma
- Foreign body
- Non-Otologic Origin
- Temporomandibular joint pain
- Referred otalgia from pharyngeal or laryngeal lesion
- Parotitis
- Dental pain
- Sinusitis
Evaluation:
Physical Examination
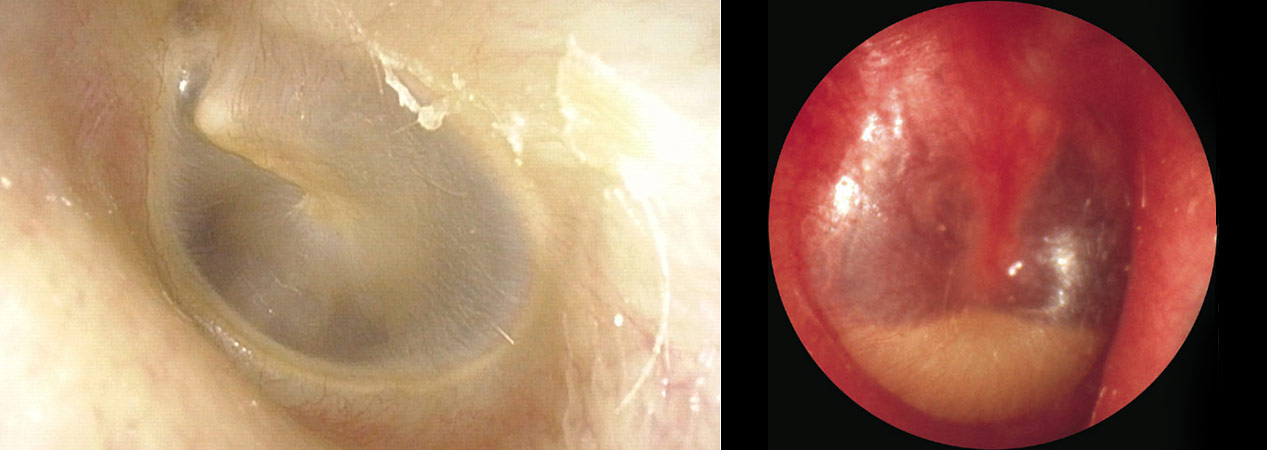
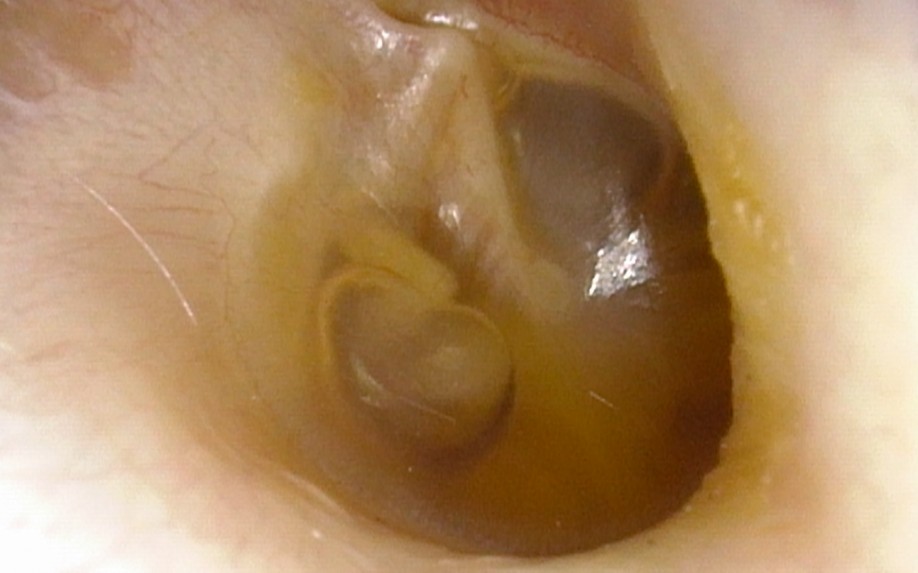
History and physical exam are usually sufficient to diagnose AOM. On pneumatic otoscopy, the tympanic membrane typically has an opaque, erythematous, bulging appearance with decreased mobility.
The immobility of the tympanic membrane distinguishes AOM from bullous myringitis, which is an isolated infection of the tympanic membrane without accompanying middle ear effusion. In advanced cases, the tympanic membrane may appear thickened and there may be exudative material or a perforation with purulent otorrhea. OME has an appearance of fluid behind the ear drum without erythema or tenderness.

Imaging Studies
Radiographic evaluation is not necessary in uncomplicated cases of AOM or OME.
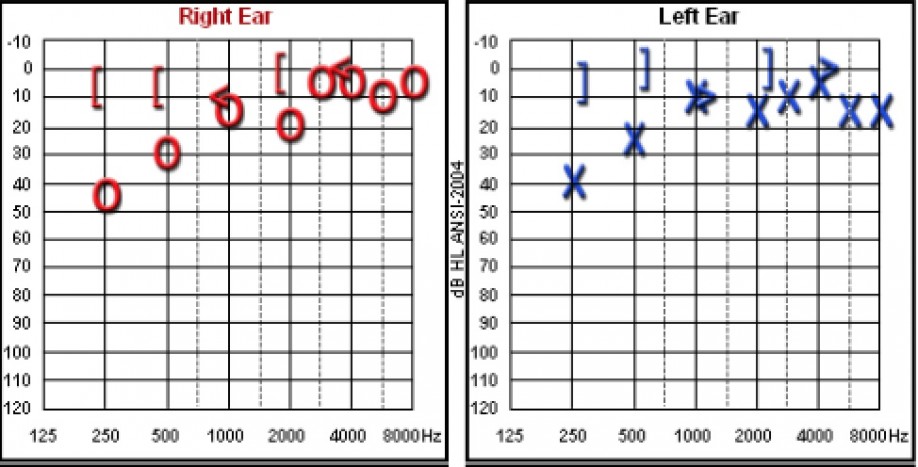
Audiometry
Audiometry is helpful for patients with persistent otitis media or effusion with concern for hearing loss. Tympanometry will also assist in determining mobility of the eardrum. Persistent fluid with conductive hearing loss should be considered for myringotomy and ventilation tubes.
Laboratory Studies
Bacterial culture is typically reserved for refractory cases of AOM or cases with complications (including acute mastoiditis). In such cases, aspiration of middle ear fluid during active infection, tympanocentesis, can be performed.

Treatment
Medical treatment of uncomplicated AOM depends on age of patient and extent of pathology. Usually uncomplicated AOM that does not resolve with observation for 48-72 hours can be treated with antibiotic therapy. For children less than 2 years of age with bilateral fluid, otorrhea or severe symptoms such as fever > 102.2 F, antibiotics are recommended. Amoxicillin or Amoxicillin-clavulanate is recommended as the first line treatment in uncomplicated acute otitis media by the American Academy of Pediatrics. Current guidelines recommend a treatment course of 10 days in patients younger than 2 years of age; this may be shortened to a 5-7 day course in older children and adults. Patients with penicillin allergy may be given Clindamycin. Analgesic and antipyretic medication should be given as adjunctive therapies for symptomatic relief. Medical treatment of otitis media with effusion involves observation as the first line. There are not enough adequate studies at this time regarding treatment of OME with steroids or decongestants to provide definitive recommendations. Antibiotics may provide short-term efficacy but is not recommended as the definitive management.
Further management involves tympanocentesis with or without tympanostomy tube placement or ventilation tubes. This procedure can be performed in the office for most adults or in the operating room for children or select adults. For AOM, tympanocentesis provides relief from fluid being extracted and provide culture fluid; however, there may be an increased risk of bleeding from the inflamed tympanic membrane. For OME, myringotomy or incision of the ear drum with tube placement will remove the fluid and may improve the conductive hearing loss.

Complications, Prognosis and Follow-Up:
In general, the prognosis for uncomplicated AOM or OME is excellent. Timely antibiotic therapy significantly reduces the risk of complications to a near-negligible level. The major complications of AOM can be divided into intratemporal, extratemporal and intracranial conditions. The most common intratemporal complication of AOM is hearing loss, which is typically a conductive hearing loss secondary to fluid in the middle ear space. Sensorineural hearing loss may occur as well, although it is a rare complication. Additional complications of AOM include perforation of ear drum, mastoiditis, labyrinthitis, petrous apicitis, facial paralysis, tympanic membrane perforation, and vestibular dysfunction.
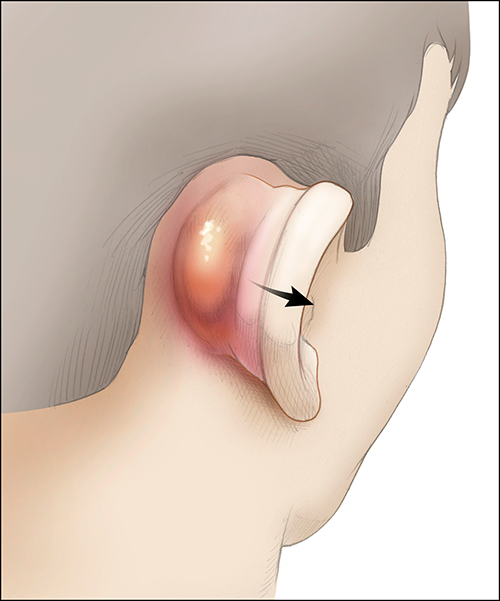
Acute mastoiditis, or inflammation of the mastoid portion of the temporal bone, is a common complication of otitis media within the temporal bone.
It is a result of direct extension of AOM. The mastoid space consists of a network of air cells and is directly connected to the middle ear via the aditus ad antrum, from which it forms during embryologic development. The incidence of mastoiditis in the US is 0.004%. Acute mastoiditis most commonly affects children between 1 and 3 years of age. Patients present with a proptotic ear, pain behind the ear, swelling behind the ear in addition to signs of otitis media. Treatment often involves intravenous (IV) antibiotics. Coalescent mastoiditis is a severe condition in which the bone of the mastoid is actively eroded by infection. Coalescent mastoiditis often requires myringotomy with ventilation tube placement, cortical mastoidectomy and IV antibiotics for adequate treatment.

Extratemporal complications are more rare. These complications involve areas of the face or neck. Examples include an abscess in the neck (“Bezold’s abscess”) or through the zygomatic root of the face(“Luc’s abscess”).
Intracranial complications are of particular concern, as they are associated with considerable morbidity; they include meningitis, subdural abscess or empyema, epidural abscess, parenchymal brain abscess, and sigmoid sinus thrombosis.
These conditions are heralded by development of neurologic symptoms such as headache, irritability, lethargy, nausea, vomiting, seizure, neck stiffness, ataxia, aphasia, or visual changes. Appropriate diagnostic radiographic imaging such as a CT with contrast or an MRI with gandolinium of the brain and temporal bone and neurosurgical consultation should be obtained if intracranial extension is suspected. Treatment involves IV antibiotics for extended periods of time. Consultation with neurosurgery for intracranial infections is important because drainage may be necessary. Sigmoid sinus thrombosis may be treated with anticoagulation in combination with antibiotics; however, this treatment is still under debate.
Patients with AOM should be monitored with regular follow up to ensure resolution of symptoms without complications. Patients with OME should also be monitored for resolution of middle ear fluid because ear tubes to improve hearing may become necessary.
Complications of Acute Otitis Media
| Category | Complications |
|---|---|
| Intratemporal | Conductive hearing loss Sensorineural hearing loss Mastoiditis Petrous apicitis Labyrinthitis Facial paralysis Vestibular dysfunction Tympanic membrane perforation |
| Extratemporal | Bezold's abscess Luc's abscess |
| Intracranial | Meningitis Subdural abscess or empyema Epidural abscess Parenchymal brain abscess Sigmoid sinus thrombosis |
Additional References
Key Points
- Acute otitis media (AOM) is defined as inflammation of the middle ear with a duration of 3 weeks or less; the most common causative bacterial organisms are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis.
- Most cases of AOM will resolve spontaneously without treatment; however, antibiotic therapy produces more rapid improvement in symptoms, promotes better resolution of effusion, and decreases the risk of complication.
- Otitis media with effusion should be treated with myringotomy and ventilation tube placement if patient has hearing loss or decreased development from ear fluid or unable to function from fluid and pressure in ears.
- Intratemporal complications include mastoiditis, labyrinthitis, petrous apicitis, sensorineural hearing loss, facial nerve dysfunction, and vestibular dysfunction.
- Acute mastoiditis without bony erosion can be treated with myringotomy with or without a pneumatization tube and IV antibiotics.
- Acute mastoiditis with osteitis or abscess requires cortical mastoidectomy, wherein the mastoid cortex is drilled down and the mastoid air spaces are opened to allow better antral drainage and ventilation.
- Intracranial complications may be life-threatening and include meningitis, subdural abscess or empyema, epidural abscess, parenchymal brain abscess, and sigmoid sinus thrombosis.