Cholesteatoma
Anatomy and Pathophysiology:
Cholesteatomas are locally destructive, squamous epithelium-lined cysts found in the middle ear or mastoid space.
They may be congenital or, more commonly, acquired. Acquired cholesteatoma may be further subdivided into primary and secondary forms. Primary acquired cholesteatoma is the most common form of cholesteatoma. Its pathogenesis is not completely understood, but a widely accepted theory is that it involves retraction of the tympanic membrane (TM). Formation of TM retraction pockets is promoted by chronic negative middle ear pressure, which can be a consequence of Eustachian tube dysfunction and chronic serous otitis media. Retraction of the TM into the middle ear space is thought to disrupt the normal self-cleaning mechanism of the ear, whereby the squamous epithelial lining of the TM and external auditory canal undergoes a lateral migratory pattern. Desquamated keratin debris becomes trapped and accumulates in the retraction pocket (cholesteatoma sac), which initiates a vicious cycle of inflammatory response and further functional physiologic impairment. Eventually, chronic infection, bony erosion, and mass effect can result, resulting in the destruction of surrounding structures.
Secondary acquired cholesteatoma is caused by the implantation of squamous epithelial material into the middle ear space as a result of tympanic membrane trauma, perforation, or surgical manipulation. It is rarely seen as a complication of tympanostomy and tympanoplasty procedures.
Congenital cholesteatoma is thought to represent an embryonic rest of epithelial tissue within the middle ear. It is diagnosed in young children who present with cholesteatoma behind an intact tympanic membrane.
Epidemiology:
Data regarding the prevalence of cholesteatoma is limited. Reports have suggested an annual incidence of 3-12 cases per 100,000 individuals. While congenital cholesteatoma is typically diagnosed in childhood, acquired cholesteatoma may be found in both adults and children. A slight male predilection has been reported.
Natural History:
Though typically slow-growing, cholesteatoma is a progressive, expansile condition that causes significant damage to surrounding structures. Bony destruction is particularly prominent and may be caused by pressure or enzyme-induced skeletal remodeling as well as up-regulation of osteoclast activity.
Presentation:
The classic symptom of cholesteatoma is painless, purulent otorrhea that is persistent or recurrent in nature. Infection of cholesteatoma is often refractory to antimicrobial therapy, due to the size and avascular nature of the mass, which impairs antibiotic delivery. Conductive hearing loss is also common as a result of accumulation keratin debris in the middle ear and erosion of the ossicles. Less commonly, patients may present with vestibular complaints due to labyrinthine involvement, or facial nerve dysfunction due to inflammation or compression. Erosion of cholesteatoma into the semicircular canals may result in complete loss of hearing.
Differential Diagnosis of Otorrhea:
- Acute otitis media
- Chronic suppurative otitis media
- Otitis externa
- Otomycosis
- Foreign body in the external auditory canal
- Cholesteatoma
- Tympanostomy tube drainage
- Malignant otitis externa
- Bullous myringitis
- Neoplasm of the external or middle ear
- Cerebrospinal fluid leak
- Traumatic middle ear hemorrhage
- Cerumen
- Inflammatory / granulomatous disease
- First branchial cleft anomaly

Evaluation:
History
History of recurrent ear infection, tympanostomy tube placement, other otologic surgery, and ear trauma should be documented. The frequency and character of otorrhea should be noted, as well as any associated symptoms suggestive of complications, such as severe headaches (although these are rare at the time of presentation).
Physical Examination
The classic description of cholesteatoma is a pearly, white mass seen through a perforation in the tympanic membrane, but the actual appearance on otoscopic examination is variable.
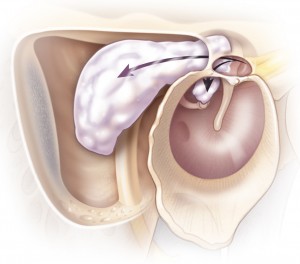
For optimal visualization, microscope examination should be performed. The most common physical findings include debris, mucopus, and granulation tissue in the external auditory canal. Tympanic membrane retraction or perforation is commonly seen in primary acquired cholesteatoma. Physical examination also includes assessment of cranial nerve function (particularly the facial nerve).
Audiology
Audiologic assessment should be performed to document the degree of conductive hearing loss.
Radiographic Studies
Radiographic imaging can be useful in determining the extent of disease and assisting in operative planning, although it is not essential in uncomplicated cases. A computed tomography (CT) scan of the temporal bone allows for evaluation of bony destruction, which is most commonly seen in the scutum and ossicles. Non-echo planar imaging (EPI) magnetic resonance imaging (MRI) is sensitive for cholesteatoma and may be used where diagnosis is uncertain or intracranial extension is suspected.
Treatment
The treatment of choice for cholesteatoma is surgical removal. In patients who are not surgical candidates, frequent microsuctioning of the ear canal with avoidance of water to minimize infection may help symptoms, but cannot stop progression.
Surgical removal is performed with the aid of an operating microscope and may be achieved through middle ear exploration and mastoidectomy as needed. The most common incision is postauricular, although the endaural approach is a common alternative.

Tympanomastoidectomy may be divided into canal wall up (CWU) and canal wall down (CWD) procedures. In CWU tympanomastoidectomy, the structure of the ear canal is preserved. Details of this approach are given in Chapter 20. The advantages of a CWU procedure are decreased risk of postoperative otorrhea and maintenance of normal ear canal anatomy. However, a second look operation is often required around one year later to ensure that there is no recurrent disease, although non-EPI MRI may be used as an alternative. The canal wall down procedure involves exteriorization of part of the mastoid. This allows for greater ease of cleaning and monitoring than the CWU procedure, and there is evidence that CWD is associated with lower rates of recurrence than CWU. Reconstruction of the tympanic membrane is performed, with reconstruction of the ossicular chain at the time of initial surgery or as a secondary procedure.
Complications, Prognosis and Follow-Up:
Untreated, complications of cholesteatoma include hearing loss from destruction of the middle or inner ear structures, facial nerve paralysis, and labyrinthine fistula. In addition, intracranial extension can result in meningitis, brain abscess, cerebrospinal fluid leakage, brain herniation, and cavernous sinus thrombosis.
The outcome for cholesteatoma following surgical removal varies depending on a number of factors, including location and extent of disease, surgical approach, and surgeon experience. Reports of overall recurrence rates range from 15-40% over 10 years. The risk of recurrence is higher in young patients and where incomplete removal of cholesteatoma is achieved.
Complications of tympanomastoidectomy include wound infection, canal stenosis, facial nerve injury, hearing loss, and vestibular dysfunction.
Long term follow up, often 10 years or more, after cholesteatoma surgery is essential. Because of the higher risk of recurrence in CWU procedures, a second-look surgery is generally advocated 6-9 months after initial tympanomastoidectomy. Although CWD procedures may reduce the risk of recurrence, the resulting mastoid bowl often requires frequent cleaning and debridement to avoid infection and otorrhea.
Key Points
- 
- Cholesteatomas are squamous epithelium-lined cysts of the middle ear and mastoid.
- Primary acquired cholesteatoma is most common and occurs as a result of Eustachian tube
dysfunction causing progressive tympanic membrane retraction and trapping of squamous
epithelium. - Cholesteatomas are locally destructive due to progressive expansion, propensity for chronic
infection, and promotion of inflammatory response resulting in bony erosion. - The classic presentation of cholesteatoma is painless, purulent, persistent otorrhea; other
symptoms include hearing loss, facial nerve dysfunction, and vestibular dysfunction. - A canal wall up tympanomastoidectomy maintains the normal ear canal and tympanic
membrane anatomy; a second-look surgery is usually recommended approximately one year
after the initial procedure. - A canal wall down tympanomastoidectomy removes part of the posterior ear canal, exteriorizing
the mastoid; lifelong frequent debridement and cleaning of the mastoid bowl in the clinic is often required as a result.

