Rhinosinusitis
Definition and Pathophysiology:
Rhinosinusitis is an infectious or inflammatory process of the nasal cavity and paranasal sinuses. An understanding of the pathophysiology of rhinosinusitis is benefited by review of sinonasal anatomy and physiology, which is discussed in Chapter 2. The interplay between infectious agent, allergens, aberrant immune reactions and disabled mucociliary clearance is important in understanding the pathophysiology of rhinosinusitis.
Rhinosinusitis can be classified based on length of time of symptoms into the following categories: acute (ARS), recurrent acute, subacute, and chronic (CRS) forms. Fungal sinusitis is considered a separate entity and is addressed in Chapter 25.
Defining Features of Rhinosinusitis
| Condition | Timing |
|---|---|
| Acute rhinosinusitis (ARS) | ≤ 4 weeks |
| Recurrent acute rhinosinusitis | ≥ 4 episodes of acute rhinosinusitis over 12-month period; complete resolution of symptoms between episodes |
| Subacute rhinosinusitis | > 4 weeks but ≤ 12 weeks |
| Chronic rhinosinusitis (CRS) | > 12 weeks |
Different expert guidelines have defined common diagnostic criteria for rhinosinusitis. The most common symptoms described include nasal congestion and obstruction, purulent posterior rhinorrhea or nasal discharge and facial pressure or pain. The Rhinosinusitis Initiative of 2004 defined major and minor criteria. Two or more major criteria or one major with two or more minor criteria are required for diagnosis of rhinosinusitis (Table: Rhinosinusitis Initiative Criteria for Diagnosis of Rhinosinusitis 2004). Diagnosis of rhinosinusitis has evolved since this criterion because studies have shown that symptoms for acute viral, acute bacteria or chronic types of rhinosinusitis are different (Table: Defining Features of Rhinosinusitis).
Rhinosinusitis Initiative Criteria for Diagnosis of Rhinosinusitis 2004
| Major Symptoms/Signs |
|---|
| • Facial pain/pressure • Facial congestion/fullness • Nasal obstruction/blockage • Nasal discharge/purulence; discolored posterior drainage • Hyposmia/anosmia • Purulence on nasal examination • Fever (acute rhinosinusitis only) |
| Minor Symptoms/Signs |
|---|
| • Headache • Fever (nonacute rhinosinusitis) • Halitosis • Fatigue • Dental pain • Cough • Ear pain/pressure/fullness |

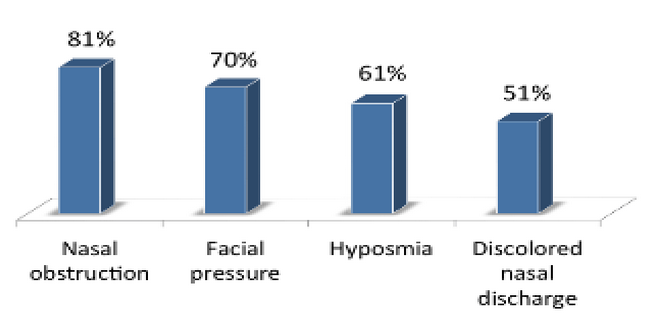
Symptom Prevalence of Chronic Rhinosinusitis 2007
ARS is defined as having a duration of less than or equal to 4 weeks. In most cases, ARS is a self-limiting viral or a bacterial infection that occurs after a viral upper respiratory tract infection (URI). The natural history of uncomplicated URI generally involves symptomatic improvement or resolution within 7-10 days after onset. In patients with acute viral rhinosinusitis, symptoms may persist for longer or up to 12 weeks. According to the 2013 European guidelines, bacterial rhinosinusitis involves at least 3 of the following symptoms: discolored discharge, severe local pain, fever, elevated ESR or CRP and “double sickening.” “Double sickening” is a worsening of symptoms after an initial improvement. The causative organisms most commonly identified in bacterial ARS are Haemophilus influenzae, Streptococcus pneumoniae, Moraxella catarrhalis, and Staphylococcus aureus.
Recurrent ARS is diagnosed in patients who have had 4 or more episodes in a 12-month period. Each episode of ARS lasts at least 7-10 days, with complete resolution between episodes. There is much research into the diagnosis and management of recurrent ARS and the possibility of this diagnosis as a variant of chronic rhinosinusitis.
Subacute rhinosinusitis refers to patients with symptoms lasting greater than 4 weeks but less than 12 weeks. It is generally regarded as a low-grade prolongation of symptoms from acute infection.
Chronic rhinosinusitis (CRS) is defined as symptoms of rhinosinusitis lasting for more than 12 consecutive weeks. Currently, CRS is predominantly thought of as an inflammatory process that may be initiated or exacerbated by a variety of host and environmental factors, including allergy, neoplasm, mucociliary dysfunction, viral/bacterial/fungal infection, trauma, irritant exposure, and medications. When present, bacterial organisms in CRS are more commonly Staphylococcus aureus, Pseudomonas aeruginosa, and other gram-negative or anaerobic pathogens. The pathogenesis of CRS is not completely understood and continues to be an active area of research and debate.
Epidemiology:
As a general condition, rhinosinusitis is extremely common, with an estimated 1 in 7 adults experiencing symptoms at some point during their lifetime. Rhinosinusitis represents the fifth-most common reason for prescription of antibiotic therapy and has been reported to account for up to $5 billion in annual health care costs. In terms of quality of life, patients have reported a worse quality of life compared to chronic disease such as congestive heart failure or chronic obstructive pulmonary disease.
Natural History:
Studies have shown that most cases of viral ARS are self-limiting and will resolve even without antibiotic therapy. Bacterial ARS often will not improve unless treated. Although progression of ARS to CRS (due to inflammatory changes initiated by a variety of etiologies) has been proposed as a potential mechanism for CRS pathogenesis, it is unclear what factors increase the risk of this occurring. The vast majority of patients who experience ARS do not go on to develop CRS.
The behavior and treatment responsiveness of CRS varies among individuals, but in general it is viewed as a persistent condition. In most cases, symptoms remain confined to the sinonasal tract; rarely, untreated CRS may extend intracranially or into the orbit, causing complications.
Presentation:
As shown in Table 24.2, the symptoms of rhinosinusitis are varied. This is particularly the case for CRS, where patient-reported symptoms have been shown to correlate poorly with radiographic extent of disease. The most common presenting symptoms in CRS are nasal discharge, nasal obstruction, facial congestion, and facial pain or pressure.
Differential Diagnosis of Rhinosinusitis:
- Infectious
- Vasomotor rhinitis
- Allergic rhinitis
- Temporomandibular joint pain
- Eustachian tube dysfunction
- Headache/migraine
- Dental pain
- Trigeminal neuralgia
- Sinonasal neoplasm
Evaluation:
History
The patient history in suspected rhinosinusitis includes timing of symptom onset and progression. It is important to investigate exacerbating events or associated symptoms. Eliciting prior treatment including over the counter medications, allergy history, exposure to irritants or inhalants, and any history of sinonasal surgery is helpful is determining severity of symptoms.
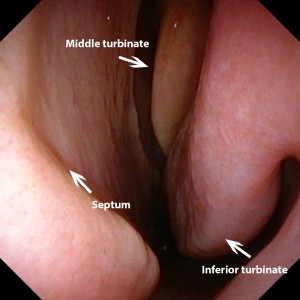
Physical Examination
The physical examination should include evaluation of the sinonasal tract via anterior rhinoscopy and rigid nasal endoscopy.
See Chapters 7 and 9 for details regarding these procedures. The presence of mucopurulent nasal drainage, inflamed or edematous nasal mucosa or nasal polyps may be seen.
Particularly in cases of CRS refractory to initial therapy, it may be beneficial to take cultures from the middle meatus to guide treatment.

Imaging Studies
Radiographic evaluation with computed tomography (CT) is indicated in cases where operative intervention is planned, when symptoms do not correlate with examination findings, if extension outside of the sinonasal tract is suspected, and, in some cases, to monitor disease progression and treatment response. CT is not recommended for initial diagnosis of rhinosinusitis. CT without contrast is the preferred modality of imaging rather than MRI because it provides superior visualization of bony anatomy, identification of mucosal thickening due to inflammation and the presence of fluid accumulation within the paranasal sinuses. Magnetic resonance imaging (MRI) is indicated where intracranial or intraorbital involvement is suspected.
Treatment
Viral ARS is typically treated with supportive care and saline irrigation. Bacterial ARS is treated with antibiotic therapy. The choice of antimicrobial agent depends on disease severity and whether the patient is likely to be at risk for antibiotic resistance (such as if antibiotics have been previously administered within the past 4-6 weeks). The first line therapy for mild cases and low risk of resistance is a 10-14 day course of amoxicillin or amoxicillin-clavulanate. Additional agents that may be considered include trimethoprim-sulfamethoxazole, ceftriaxone, or fluoroquinolones. Treatment failure is an indication for nasal cultures.

Chronic rhinosinusitis management involves both medical and surgical interventions. Effective treatment regimens are topics of active research. Currently, medical management begins with nasal saline irrigations. Multiple randomized controlled trials have shows improvement of patient symptoms and endoscopy scores with regular, high volume (100 ml or more) of saline. Nasal steroid sprays have also shown in randomized studies to be effective. However, the type of nasal steroid and dose is still debated. Generally, doses that are reported to be effective are higher than doses used over the counter. In addition, many otolaryngologists utilize oral steroids or chronic antibiotics. In Europe, 3-4 week courses of macrolides are recommended. However, the macrolide reported to be effective is not approved for use in the US. In the US, oral steroids are frequently used in addition to saline irrigations or short 10-14 day courses of antibiotics. Furthermore additional investigation into allergic or immunologic etiology may be warranted in patients who are resistant to treatment despite high compliance.

Maximal medical therapy is generally defined as 4-6 weeks of saline irrigation, appropriate antibiotic therapy and steroid treatment. Failure of maximal medical therapy is an indication for functional endoscopic sinus surgery (FESS) (See Chapter 27). The principle underlying FESS is the restoration of normal mucociliary flow by addressing anatomic deficiencies. This includes techniques that widen the natural maxillary sinus ostium or obliterate the ethmoid air cells in order to promote sinus drainage. Surgery is also indicated in cases of intraorbital or intracranial extension from complications of rhinosinusitis.

Complications, Prognosis and Follow-Up
The most concerning complications of rhinosinusitis include orbital and intracranial involvement. These complications are rare in acute and chronic rhinosinusitis, but common in invasive fungal sinusitis. Orbital extension of infection can produce orbital cellulitis, subperiosteal abscess, orbital abscess, or cavernous sinus thrombosis. Intracranial extension can lead to meningitis or epidural abscess. Pott’s puffy tumor is a complication of frontal sinus infection, wherein osteomyelitis of the frontal bone results in swelling of the forehead that must be surgically drained and debrided. Other local complications of rhinosinusitis include mucocele formation with bony erosion, which is most concerning in the frontal, sphenoid, and ethmoid sinuses.
Most patients undergoing FESS report improvement in symptoms, with documented success rates as high as 90%. However, many patients may continue to require medical therapy on an intermittent or continual basis or repeat surgery to address persistent or recurrent symptoms.
Additional References
Key Points
- Temporally, rhinosinusitis is separated into acute (ARS; up to 4 weeks), recurrent acute, subacute, and chronic (CRS, over 12 weeks) forms, along with acute exacerbation of chronic rhinosinusitis.
- The causative organisms most commonly identified in ARS are Haemophilus influenzae, Streptococcus pneumoniae, Moraxella catarrhalis, and Staphylococcus aureus.
- The most common bacterial organisms isolated in CRS are Staphylococcus aureus, Pseudomonas aeruginosa, and other gram-negative or anaerobic pathogens.
- Viral ARS is treated with supportive care. Bacterial ARS is treated with antibiotic therapy; amoxicillin is a first-line agent.
- Maximal medical management of CRS entails 4-6 weeks of culture-directed antibiotics with corticosteroids; failure of maximal medical therapy and extension of disease outside the sinonasal tract are indications for functional endoscopic sinus surgery (FESS).
- Orbital complications of rhinosinusitis may include orbital cellulitis, subperiosteal abscess, orbital abscess, or cavernous sinus thrombosis.