Audiology
Audiology provides formal measures of the auditory system resulting in diagnostic information regarding the type and magnitude of hearing loss, as well as its functional impact on the patient. These include behavioral measures such as pure tone audiometry and speech testing, physical measures such as tympanometry, and physiological measures such as auditory acoustic stapedial muscle reflexes, auditory brainstem responses, and otoacoustic emissions. Taken together, the results quantify auditory dysfunction, anatomically localize the sources of the problem, and provide etiology information. Additionally, in many cases, they also assist in monitoring disease progression, guide the approach to therapy, and quantify intervention effectiveness.
Pure Tone Audiometry
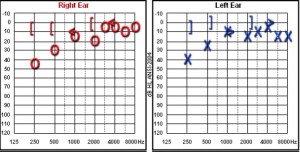
The most commonly used audiologic measure is the pure tone audiogram. In this procedure, the thresholds of hearing are determined for individual pure tones of varying frequency (pitch). The normal frequency range of human hearing is from 20 to 20,000 Hz; most audiograms show results in the 250-8,000 Hz range, where the majority of speech occurs. The lowest level of sound at which a patient is able to detect 50% of a series of presentations at a single frequency is referred to as the threshold for that particular frequency. The threshold values for the individual frequencies are recorded on a graph.
The stimulus tones in pure tone audiometry are administered to each ear separately to enable function to be evaluated independently on each side. The stimuli are presented via earphones (air conduction) and again through a vibratory device placed over the forehead or mastoid process (bone conduction). The threshold values for each method are plotted separately. Comparison of the threshold data between the two methods (air-bone gap) can identify whether hearing loss is conductive, sensorineural, or mixed. If the air conduction thresholds and bone conduction thresholds are equivalent or only minimally different (air-bone gap of < 10 dB), there is no conductive component and the hearing loss is sensorineural. Conversely, if the air conduction thresholds are greater than the bone conduction thresholds (air-bone gap of >10 dB), the hearing loss is conductive. In conductive hearing loss, the bone conduction thresholds are within normal limits, but the air conduction thresholds are abnormal, with a 10 dB air-bone gap or greater. Mixed hearing loss is also characterized by a 10 dB or greater air-bone gap, but with both air and bone conduction thresholds in the abnormal range.
The pure tone average (PTA) is the average of the threshold values at the standard frequencies of 500, 1000, 2000 and 3000 Hz. Because these frequencies span the range that encompasses speech production, the PTA provides an estimate of functional impairment.
The severity (degree) of hearing loss can be graded based on the PTA (or the hearing threshold for a different frequency range). One classification system is summarized in Table 3.1.
| Threshold Intensity | Degree of Hearing Loss |
|---|---|
| -10-15 dB | Normal |
| 16-25 dB | Slight |
| 26-40 dB | Mild |
| 41-55 dB | Moderate |
| 56-70 dB | Moderately severe |
| 71-90 dB | Severe |
| >90 dB | Profound |
Speech Audiometry
Measures of speech threshold and speech recognition are useful adjuncts to pure tone audiometry and provide information regarding functional impact of auditory impairment. The speech stimuli are presented with standardized recordings or with live voice. The results of speech audiometry should correspond with the pure tone results.
One type of speech audiometry measures the threshold level for speech, usually in the form of bisyllabic words. The speech reception threshold (SRT) is the threshold level (in dB) at which a patient can correctly understand and repeat 50% of a series of the words . The speech awareness threshold (SAT) is like the SRT, but the patient needs only to recognize that the words are present rather than understand the words.
Unlike pure tones, the speech stimulus is composed of a range of frequencies primarily within the 500-2000 Hz range. Therefore, a patient may have a normal SRT or SAT despite a significant hearing loss at frequencies below 500 Hz or above 2000 Hz. In such cases, the speech threshold may not be a true indicator of function, as such a patient would likely have difficulty understanding conversation in a practical setting (such as with substantial background noise). However, speech threshold values are useful as a check of the validity of the PTA.
A second type of speech audiometry measures the ability to understand speech (usually in the form of monosyllabic words) presented at a suprathreshold level, typically 40 dB above the patient’s SRT. The word recognition score (WRS; also known as a speech discrimination score) is the percentage of words correctly identified from a list of 50 or 25 words. The WRS provides data regarding a patient’s functional capacity because it more closely approximates a real life speech communication scenario.
Immittance Measures
Acoustic immittance measures include tympanometry and acoustic middle ear muscle reflex testing. They provide information regarding the function of the tympanic membrane and middle ear, as well as the integrity of the acoustic reflex pathway.
Tympanometry is performed by measuring the level of a tone reflected by the tympanic membrane. A stimulus tone (usually 226 Hz) is applied via a probe inserted snugly into the external auditory canal, thereby sealing the canal and allowing for measurement of reflected sound. The device measures the amount of sound in the external ear canal, which depends on the acoustic characteristics of the tympanic membrane. These acoustic characteristics determine how much sound is reflected or absorbed and vary according to the physical characteristics of the tympanic membrane itself (such as compliance), the characteristics of the middle ear, and the pressure difference between the ear canal and the middle ear air space. The measurement produces a tympanogram, or graph of acoustic characteristics (immittance) versus applied air pressure. Based on this graph, the volume of the ear canal, the air pressure in the middle ear space, and amount of sound transmitted into the middle ear can be determined. The greatest amount of sound absorption by the tympanic membrane occurs when ear canal air pressure and middle ear air pressure are equivalent; this is represented by a peak in the graph. Under normal circumstances, the Eustachian tube equalizes the air pressure in the middle ear space with the outside environment, so the peak pressure occurs near 0 daPa. If, however, the middle ear space is inadequately aerated due to Eustachian tube dysfunction, the tympanometric peak occurs at a negative air pressure. In contrast, a flat tympanogram can result either when a middle ear effusion is present or if the tympanic membrane is perforated (or contains a pressure equalization tube). The two cases can be distinguished based on the calculation of ear canal volume that will be abnormally large with a tympanic membrane perforation but within the normal range if the tympanic membrane is intact. Certain other conditions of the middle ear, such as ossicular discontinuity and otosclerosis, produce changes in the amplitude of the tympanogram’s peak.
The acoustic stapedius muscle reflex is a physiologic response that may serve to mitigate loud sounds reaching the cochlea. When a loud sound stimulus is applied, the stapedius muscle contracts, causing stiffening of the ossicular chain and decreased compliance of the tympanic membrane. This reduces the level of the sound transmitted to the cochlea. An intact reflex requires transmission of the loud stimulus to the cochlea and brainstem (i.e., cochlear, auditory nerve, and brainstem function must be intact), as well as a functional stapedius muscle (innervated by cranial nerve VII) and normal middle ear components. Normally, a stimulus applied to one ear produces bilateral stapedius muscle contraction. Acoustic reflex measures determine the threshold (softest level) at which the reflex is triggered (measured in the same manner as tympanometry, based on tympanic membrane characteristics). The ipsilateral and contralateral acoustic stapedius reflex thresholds vary depending on the magnitude and type of auditory dysfunction. Results of acoustic reflex testing based on etiology of dysfunction are summarized below.
| Disorder | Ipsilateral Reflex | Contralateral Reflex |
|---|---|---|
| Mild or moderate SNHL (unilateral or bilateral), stimulus applied to either ear | Present | Present |
| Unilateral CHL or severe to profound SNHL, stimulus applied to affected ear | Absent | Absent |
| Unilateral CHL or severe to profound SNHL, stimulus applied to normal ear | Present | Absent |
| Bilateral CHL or severe to profound SNHL, stimulus applied to either ear | Absent | Absent |
| Unilateral CN VIII lesion, stimulus applied to affected side | Absent | Absent |
| Unilateral CN VIII lesion, stimulus applied to normal side | Present | Present |
| Unilateral CN VII lesion (affecting stapedius function), stimulus applied to affected side | Absent | Present |
| Unilateral CN VII lesion (affecting stapedius function), stimulus applied to normal side | Present | Absent |
| Central brainstem lesion, stimulus applied to either ear | Present | Absent |
Auditory Brainstem Response
The auditory brainstem response (ABR) evaluates the function of the peripheral ear (external ear, middle ear and cochlea) and the auditory nerve, brainstem, and midbrain. The measures involve auditory stimuli and the measurement of electrical signals from surface electrodes, similar to those used for electroencephalography (EEG). Under normal conditions, application of a sound stimulus produces a characteristic series of electrical waves (auditory evoked potentials) generated within 10-15 milliseconds after the stimulus is applied, which can be recorded from electrodes placed on the scalp. The first two waves are generated from the auditory nerve, while the following three waves are produced by the brainstem and midbrain. Abnormalities in the latencies of the various waves (both in relation to the time of stimulus as well as to the preceding wave in the sequence) can assist in localizing dysfunction to particular portions of the retrocochlear auditory pathway. An alternative use for ABR is to determine the auditory thresholds for patients who are unable to cooperate with instructions necessary to perform PTA. In this case, the threshold (softest level) necessary to elicit an ABR is determined for each frequency via both air and bone conduction. As they do not require any voluntary response on the part of the patient, ABR measures are commonly used to assess hearing loss in newborns or in any other patients for whom voluntary responses are not possible.
Otoacoustic Emissions
Otoacoustic emissions (OAE) are sounds originating from the movement of the outer hair cells of the cochlea when stimulated. A sensitive microphone placed in the ear canal can detect these sounds and provide information regarding cochlear pathology. For instance, in sensorineural hearing loss, the presence of normal OAE indicates normal cochlear function, suggesting the presence of retrocochlear pathology (such as auditory nerve or central dysfunction). However, although OAE are generated by the cochlea, a moderate conductive hearing loss due to outer or middle ear pathology may decrease cochlear stimulation sufficiently to eliminate OAE and may also reduce the sound level coming from the cochlea back into the ear canal, even if cochlear function is normal. OAE are also often used to screen for hearing loss in the neonatal population.
Key Points
- Pure tone audiometry determines the threshold (softest intensity) at which a patient can detect a range of individual frequencies; thresholds are determined for each ear separately with stimuli applied via air conduction and bone conduction.
- Speech audiometry determines the speech threshold and word recognition score. It validates the results of pure tone audiometry and provides information regarding the functional impact of hearing impairment.
- Tympanometry is a measure of tympanic membrane characteristics; negative middle ear pressure due to Eustachian tube dysfunction, the presence of middle ear effusion or tympanic membrane perforation, or pathology of the ossicular chain can all cause characteristic changes in tympanogram morphology.
- The acoustic reflex measures the change in tympanic membrane compliance due to contraction of the stapedius muscle in response to loud sound stimulus; the reflex requires a functional stapedius muscle and is normally produced in both ears. The pattern of acoustic reflex response can assist in localization of auditory dysfunction.
- The auditory brainstem response (ABR) consists of characteristic electrical responses (waves) generated by the auditory nerve, brainstem, and midbrain approximately 10-15 milliseconds after a sound stimulus is applied; ABR can be used to localize retrocochlear pathology or as an alternative to pure tone audiometry for patients who cannot cooperate with instructions.
- Otoacoustic emissions (OAE) are sounds produced by movements of the outer cochlear hair cells in response to sound stimulation and can be used to distinguish cochlear from non-cochlear pathology, or as a screening tool for hearing loss.